HIV and Your Sexual Health


HIV and Your Sex Life
HIV doesn’t mean your sex life is over. There are lots of emotional and physical perks to having sex. It can reduce stress, improve your mood, and even boost your heart health! But you’ll need to take care of your sexual health and do what you can to help protect your partners. Here’s what you need to know.

Be Honest About HIV
Before you have sex, let your partner know that you have HIV. That might seem hard, but being honest about your health lets them make an informed choice. It also protects you. Under some state laws, you have to disclose your HIV status before you have sex with a new partner.

Tell Your Doctor
From primary care doctors to OB/GYNs and urologists, lots of different health care providers can support your sexual health. Make sure any doctor you see is aware of your HIV status. That way, they can schedule tests and shots you need to stay healthy and prescribe drugs that are safe to take with your HIV treatment. They can also take extra steps so they don’t come into contact with your blood or other body fluids.

Stay on Top of Your Treatment
Antiretroviral therapy (ART) lowers the level of HIV in your blood. After several months, the virus may no longer show up on a blood test. At that point, you can’t transmit HIV to your partner during sex. Once your HIV is undetectable, stick to your treatment plan. If not, the virus could build up in your bloodstream again and put your partners at risk.

Get Screened
HIV is not the only STI you need to think about. If you are sexually active, you continue to run the risk of exposure to other STIs like gonorrhea, chlamydia, herpes, and syphilis. HIV makes these infections harder to treat, so use condoms to lower your risk, and get screened for STIs at least once a year.

Get Your Shots
Vaccines can prevent some STIs, including hepatitis A and B and human papillomavirus (HPV), which causes several kinds of cancer. Talk to your doctor if you’ve not sure whether you’ve had these shots. They will recommend vaccines based on your age, vaccines you’ve already had, and other risk factors.

Don’t Put Off Your Yearly Pap Test
Women who live with HIV are six times more likely to get cancer in their cervix, the lower part of your uterus that connects to your vagina. The HPV vaccine can help protect you from cervical cancer. Routine Pap tests, in which a specialist looks at cells from your cervix under a microscope, can catch cervical cancer in its earliest stages or even before it starts. The earlier it’s found, the easier it is to treat.

Wear a Condom
Even if you use another type of birth control, wear a condom or dental dam when you have vaginal, anal, or oral sex. It’s the only way to protect against HIV and other STIs. Choose a water or silicone-based lube to keep the condom from slipping. Skip oil-based lube like petroleum jelly or massage oil – it can weaken the condom and cause it to break.

Find Less Risky Ways to Have Sex
You’re most likely to pass HIV on to a partner through anal or vaginal sex. Hook up in ways that aren’t so risky. Oral sex doesn’t bring nearly the same level of risk. You can also explore ways to fool around that don’t involve swapping fluids like semen, vaginal fluid, or blood.

Get Help With Your Erection
As many as 60% of men with HIV can’t get or keep an erection. Talking about it with your doctor may feel awkward, but they can suggest ways to help. Sometimes changing your treatment plan can make a difference. You could also get a prescription for medicine that helps you get hard before sex.
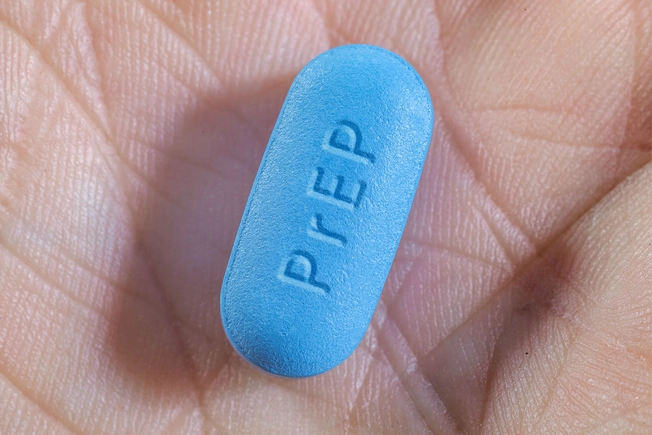
Talk to Your Partner About PrEP
Pre-exposure prophylaxis (PrEP) is a drug that can protect your partner from getting HIV from you. A doctor can prescribe it as a pill or as a shot. After 7 days of pills, your partner will be fully protected during anal sex (bottoming.) After 3 weeks, they’ll be protected during vaginal sex. But to get this protection, your partner must take the medicine exactly according to their doctor’s directions.

Know How to Get PEP
If your condom breaks or if your blood tests are still picking up HIV, your partner can protect themselves after sex. A series of pills called post-exposure prophylaxis (PEP) can stop HIV from spreading through their body. They’ll need to act fast though. To stop the virus, your partner has to start PEP within 72 hours (3 days) after sex. They can get PEP from a doctor, health clinic, or hospital ER.
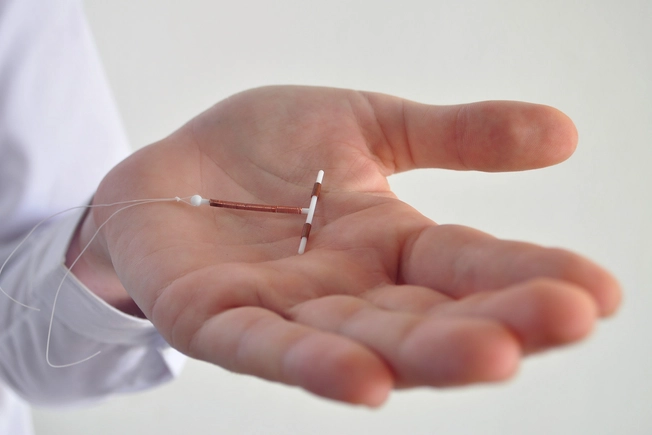
Find the Right Type of Birth Control
HIV drugs affect how well some forms of birth control work, like pills, implants, and shots. If you don’t want to get pregnant, you may need to use a different or second type of birth control. Talk to your doctor about your options. If your partner has HIV too, a diaphragm or IUD is often the safest choice.

Plan for a Family
If you’re thinking about having a baby, ask your doctor about the pros and cons of taking HIV drugs when you’re pregnant. Also find out how you can protect your baby from HIV during pregnancy, delivery, and breastfeeding. And adopting or using a surrogate are other choices you can explore. It is illegal for adoption agencies to discriminate based on applicants’ HIV status.

Talk About Your Sex Life
Problems with sex can be really common when you live with HIV. At some point, you might lose interest, have trouble getting aroused or erect, or not be able to orgasm. If your doctor has ruled out other health issues, think about therapy. Talking to a counselor could help recharge your sex life.
IMAGES PROVIDED BY:
Maria Botina / EyeEm / Getty Images
Carlina Teteris / Getty Images
Thomas Barwick / Getty Images
Francis Sheehan / Science Source
Stefania Pelfini, La Waziya Photography / Getty Images
SimpleImages / Getty Images
Anchalee Phanmaha / Getty Images
Rattanakun Thongbun / EyeEm / Getty Images
Catherine Falls Commercial / Getty Images
Courtney Hale / Getty Images
MarcBruxelle / Getty Images
Guido Mieth / Getty Images
flocu / Getty Images
Luis Alvarez / Getty Images
Maskot / Getty Images
SOURCES:
HIV.gov: “Sexually Transmitted Infections,” “Talking about your HIV status,” “Preventing Sexual Transmission of HIV.”
HIVInfo.NIH.gov: “HIV and Immunizations,” “HIV and Women,” “HIV and Birth Control.”
CDC: “Screening Recommendations and Considerations Referenced in Treatment Guidelines and Original Sources,” “Protecting Others,” “Condom Fact Sheet In Brief,” “Protect Others If You Have HIV,’ “Family Planning,” “Telling Others,” “PrEP Effectiveness,” “On-Demand PrEP.”
Terrence Higgins Trust: “Viral load and being undetectable.”
NAM/AidsMap: “Erectile dysfunction and HIV,” “Sexual dysfunction and HIV.”
ESMO: “First Global Estimates of Cancer Attributable to HIV.”
World Health Organization: “Cervical Cancer.”
Mayo Clinic: “Cervical Cancer.”
Department of Veterans Affairs: “Birth Control and HIV.”
Planned Parenthood: “What is PEP?”
Cleveland Clinic: “5 Benefits of a Healthy Sex Life.”